Infections by the human papillomaviruses (HPV) are the most prevalent sexually transmitted infections globally. While most infections tend to be asymptomatic and usually resolve on their own, some HPV types can be very problematic. There are two main types of HPV, the low and the high-risk HPV. Certain low-risk HPV can cause anal, genital, and oropharyngeal warts, but infections with high-risk HPV can lead to genital, anal, and oropharyngeal cancers (1,2).
Cervical cancer is one of the most frequent cancers diagnosed and a leading cause of cancer death in women and people with a cervix globally and it is almost entirely caused by infections with high-risk HPV types (1). Luckily, cervical cancer is also a vaccine-preventable cancer (3).
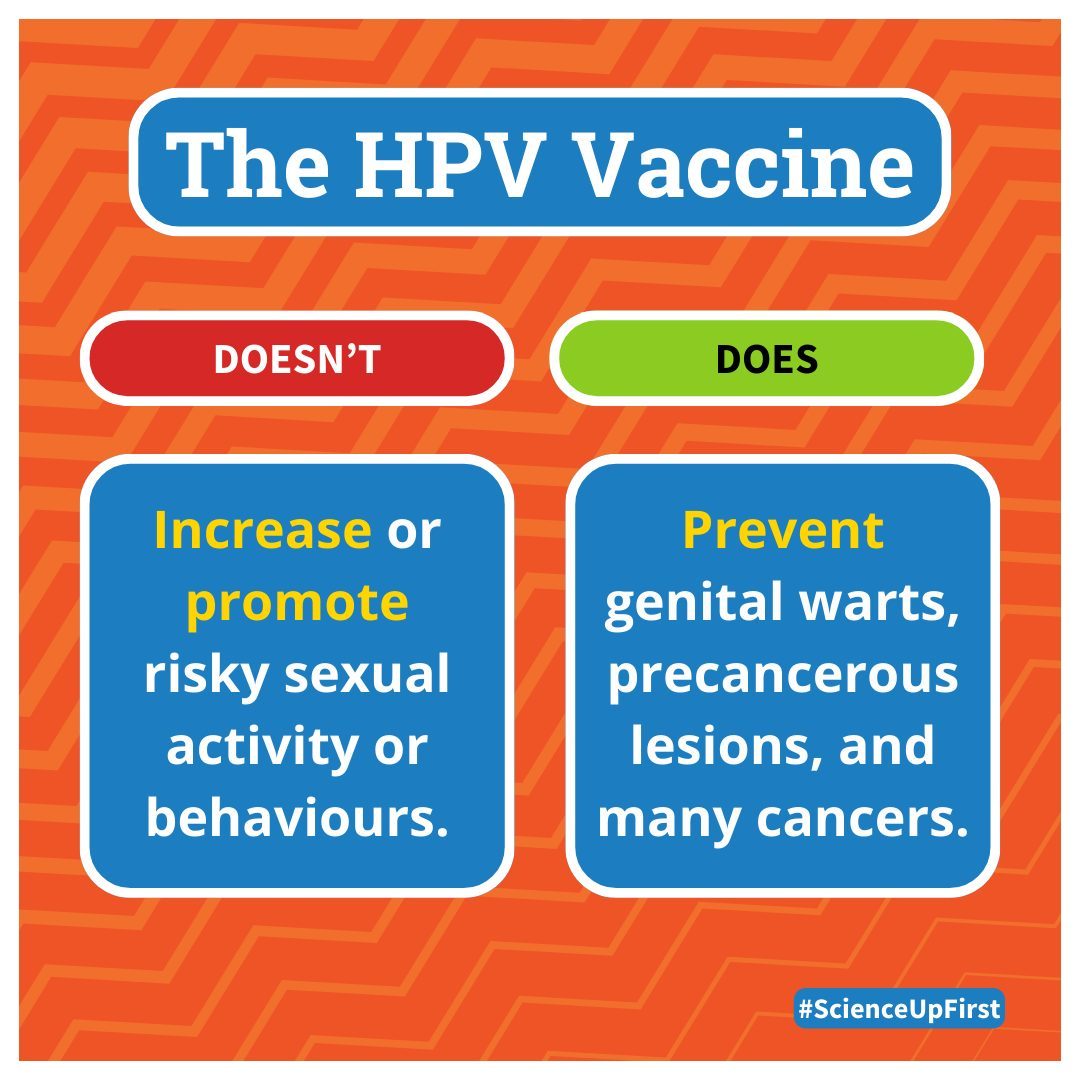
While the HPV vaccine has proven to be highly effective at reducing the risk of developing cervical cancer (4,5,6,7,8,9,10,11), there are still misconceptions about it (12,13). One belief is that it encourages risky sexual behaviors such as earlier, more frequent, and unprotected sexual activities (14,15).
This is untrue.
In fact, evidence strongly shows that HPV vaccination does not encourage sexual activity or risky sexual behaviors (14,16,17,18,19,20,21,22,23,24).
Administering the HPV vaccine at a younger age only allows for a stronger immune response and protection against disease – it has no effect on when or how someone chooses to become sexually active (16,25).
Sources: https://tinyurl.com/SUFHPVVaxAndSex
Share our original Tweet!
Infections by the human papillomaviruses (HPV) are the most prevalent sexually transmitted infections globally.
— ScienceUpFirst | LaScienced'Abord (@ScienceUpFirst) April 24, 2024
You can learn more about protection from HPV over here https://t.co/lccZnqAE7F
Got a question about HPV or other STIs? Shoot us a DM#ScienceUpFirst pic.twitter.com/WIQdR7Xn6v
View our original Instagram Post!