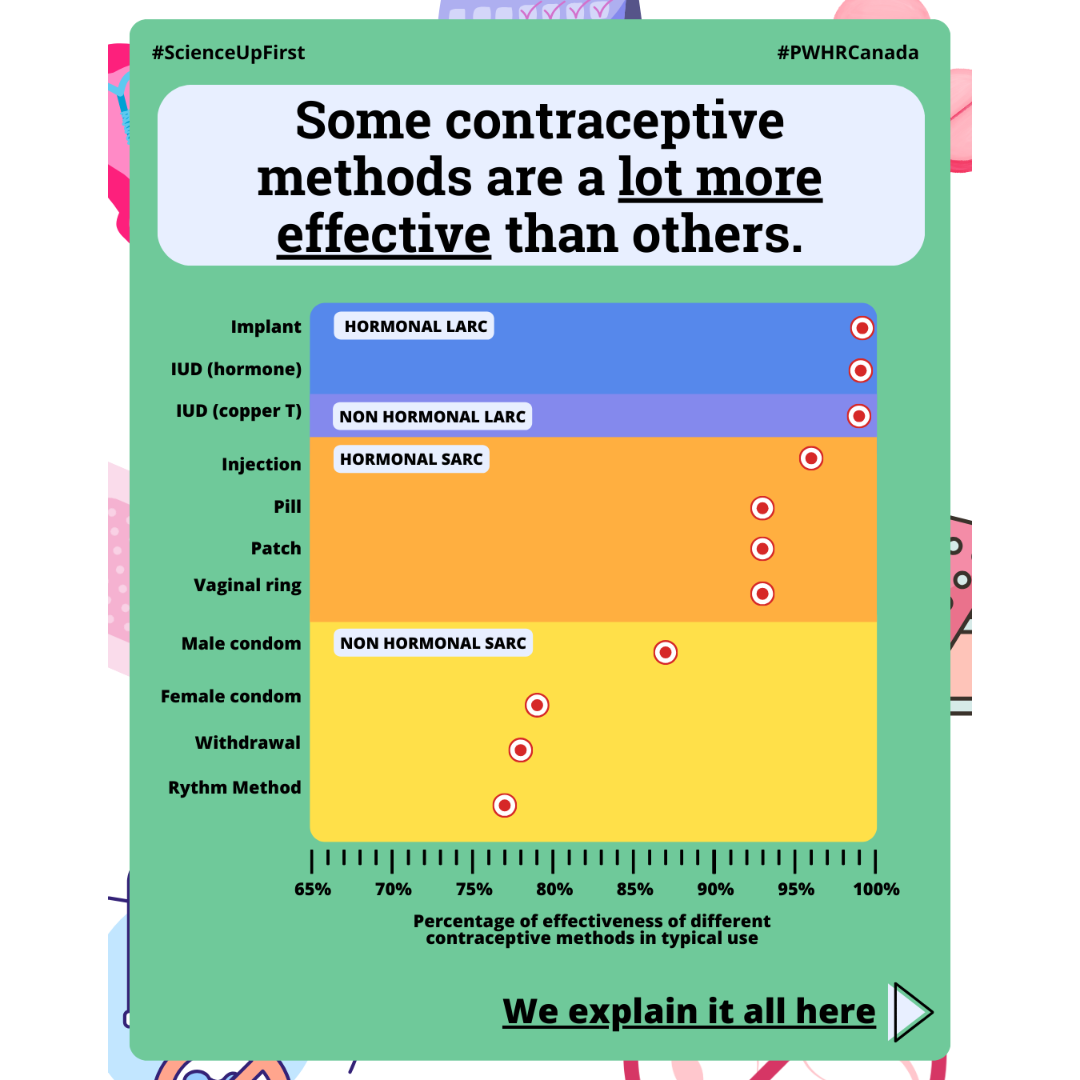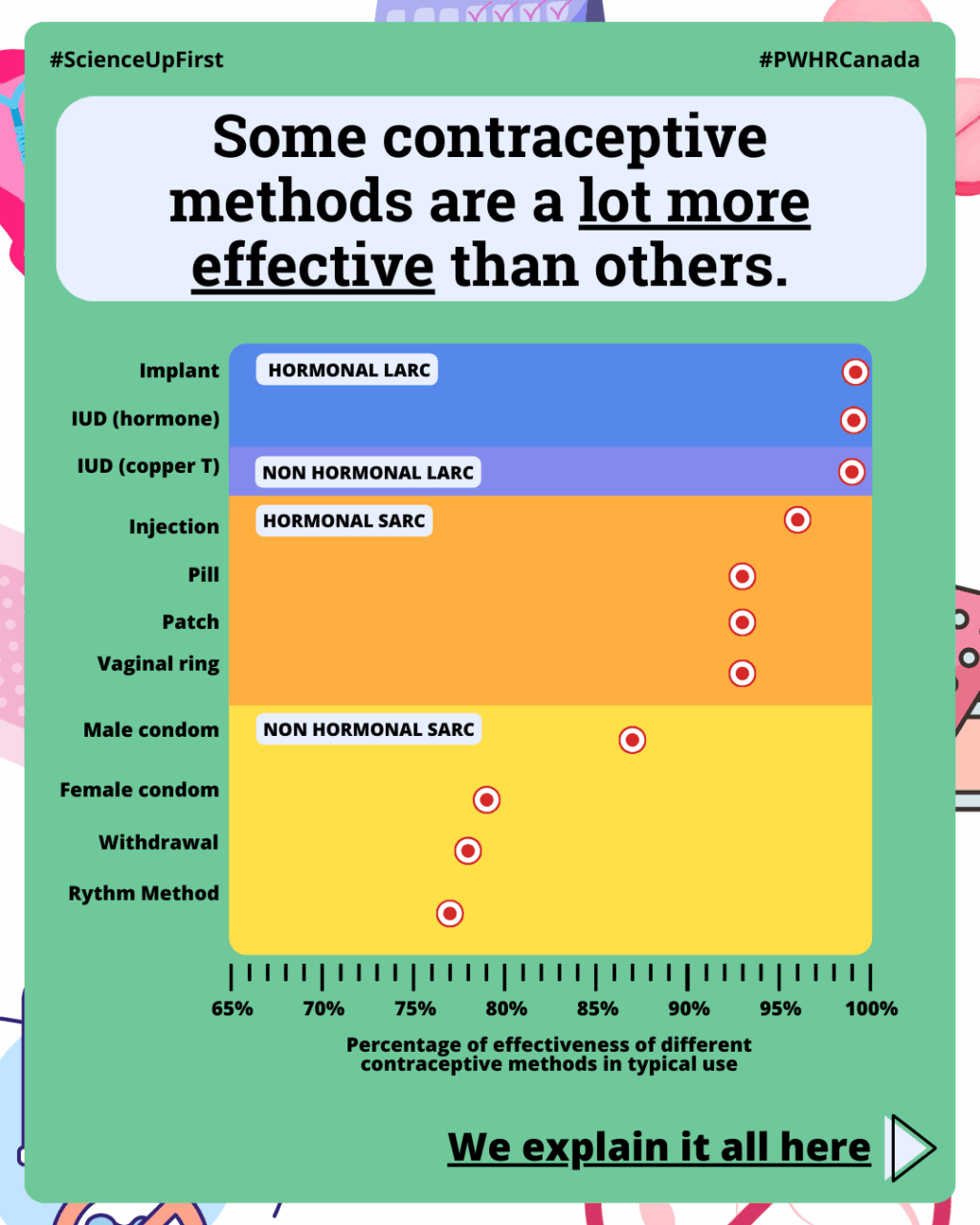
Some contraceptive methods are a lot more effective than others
Let’s go over them →
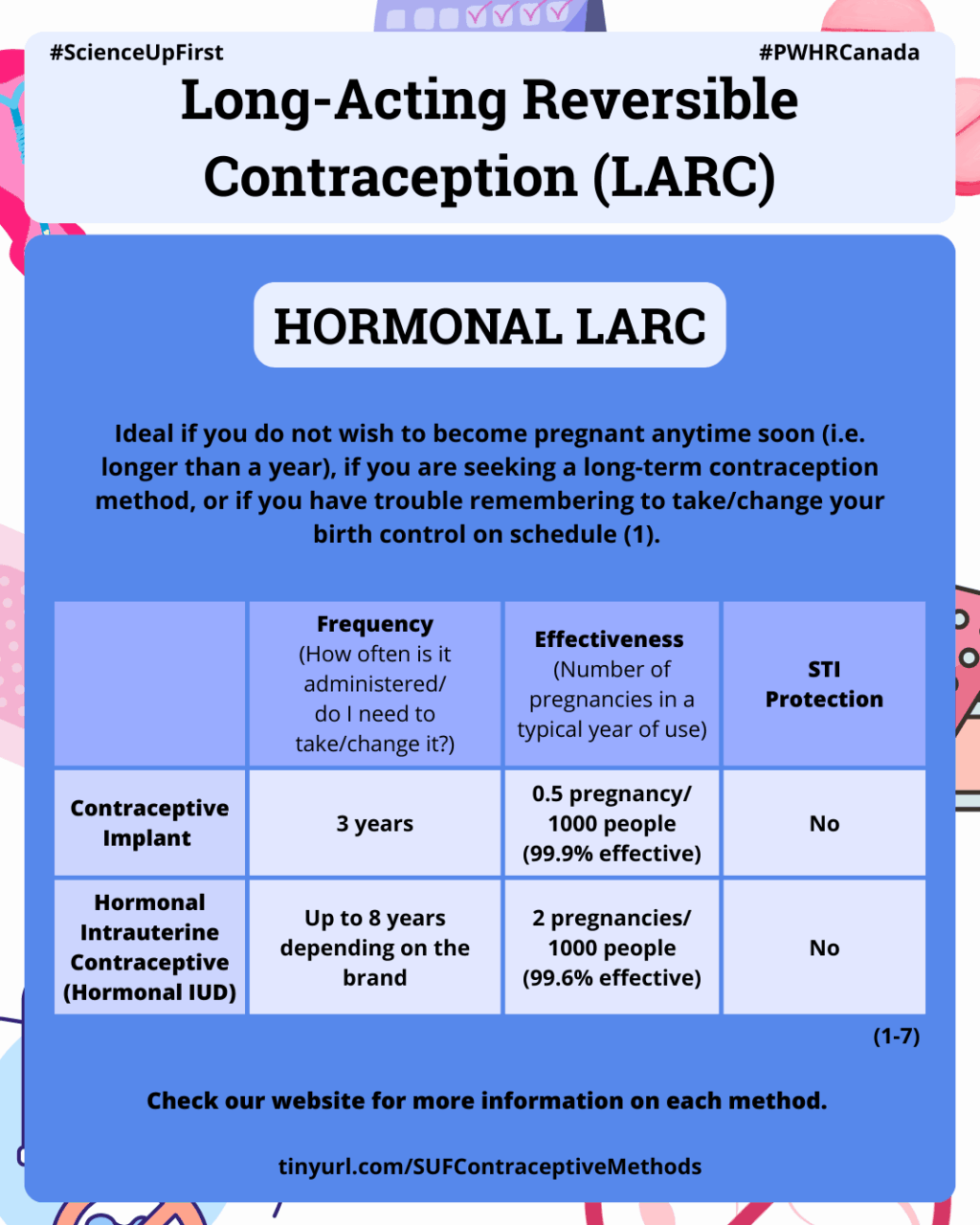
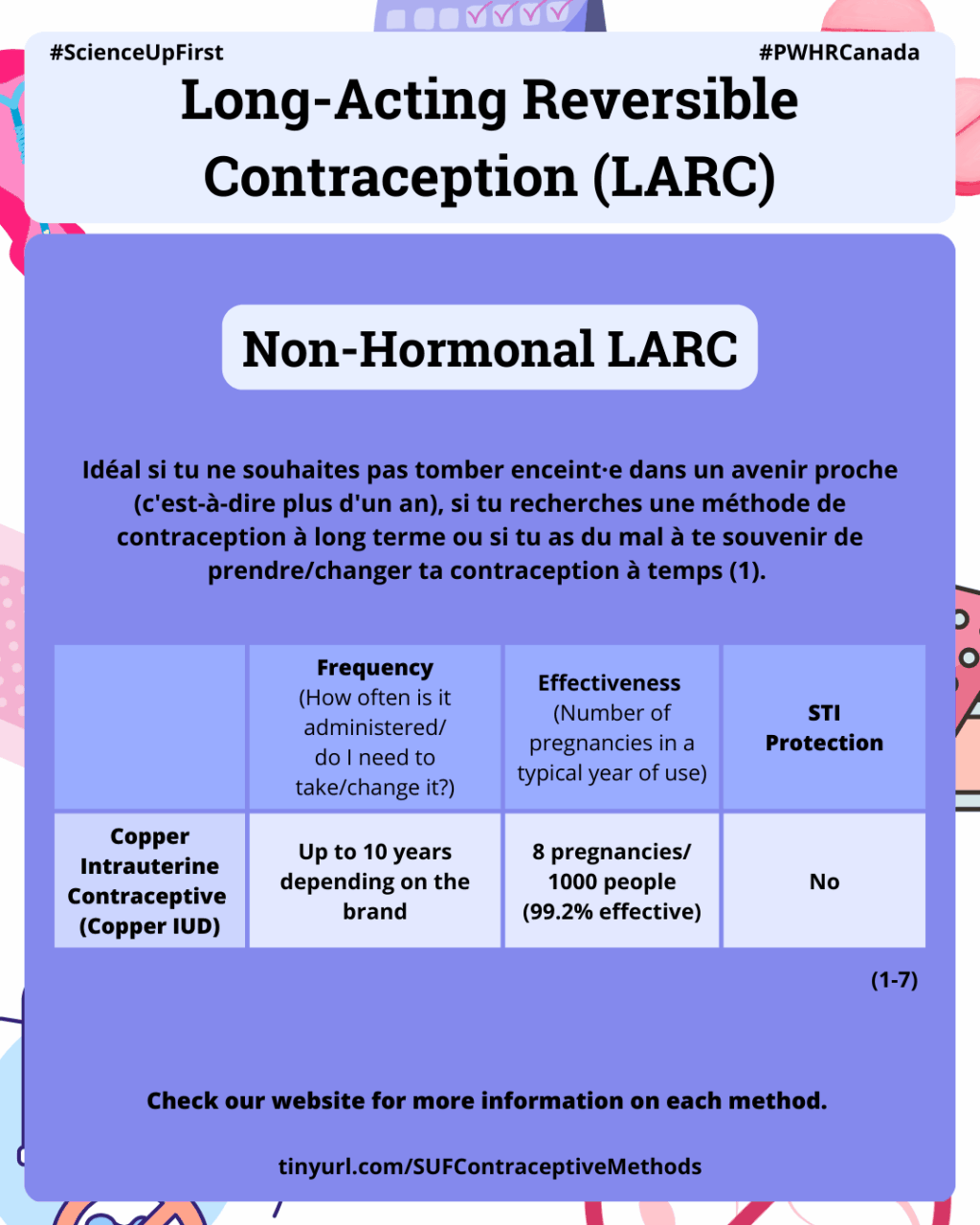
Long-Acting Reversible Contraception (LARC)
Ideal if you do not wish to become pregnant anytime soon (i.e. longer than a year), if you are seeking a long-term contraception method, or if you have trouble remembering to take/change your birth control on schedule (1).
Hormonal LARC
Contraceptive implant (4,7,8,9)
Frequency: Should be replaced every 3 years
Effectiveness with typical use: 0.5 pregnancy per 1000 people in a year (99.9% effective).
What: A soft, flexible rod inserted under the skin of your upper arm.
How: Slowly releases progestin (a hormone), which prevents the release (ovulation) of eggs (ovules) and thicken mucus in the cervix (the opening of the uterus), blocking sperm from reaching and fertilizing an ovule.
Sexually Transmitted Infection (STI) protection: No
Reversible: Yes, can be removed at any time.
Hormonal Intrauterine Contraceptive (Hormonal IUD) (6,7,8,10,11)
Frequency: Can stay in place for up to 8 years, depending on the brand.
Effectiveness with typical use: 2 pregnancies per 1000 people in a year (99.6% effective).
What: Small T-shaped device inserted in the uterus.
How: Slowly release progestin to thicken the cervical mucus preventing sperm from reaching an ovule. It also makes the lining of the uterus thinner, and can, in some cases, prevent the release of ovules (ovulation).
STI protection: No
Reversible: Yes, can be removed at any time.
Non-Hormonal LARC
Copper Intrauterine Contraceptive (Copper IUC) (4,7,11,12,13)
Frequency: Can stay in place for up to 10 years, depending on the brand.
Effectiveness with typical use: 8 pregnancies per 1000 people in a year (99.2% effective).
What: Small T-shaped device made of plastic and copper that is inserted in the uterus.
How: The released copper interferes with sperm’s movement preventing them from reaching and fertilizing an ovule.
STI protection: No
Reversible: Yes, can be removed at any time.
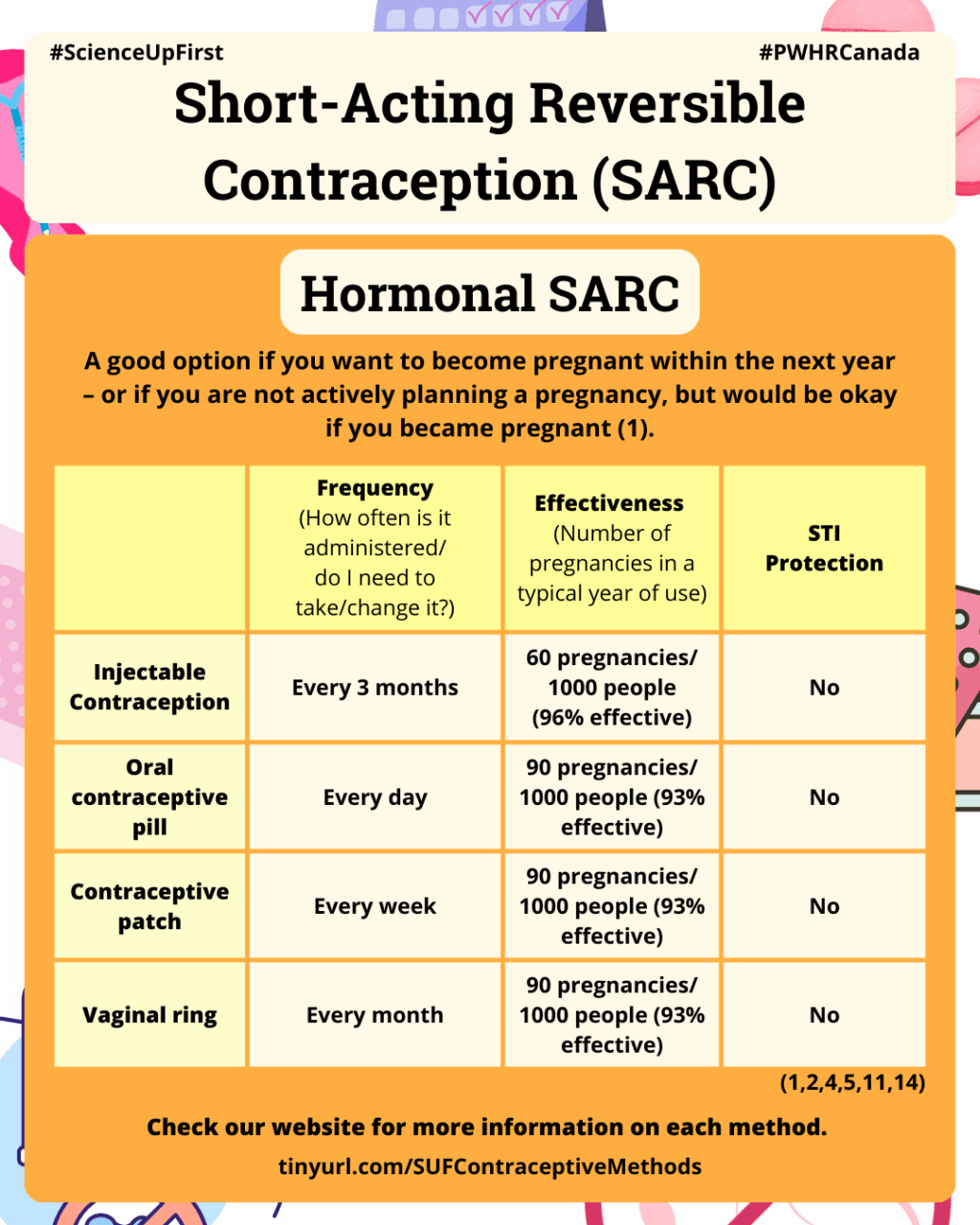
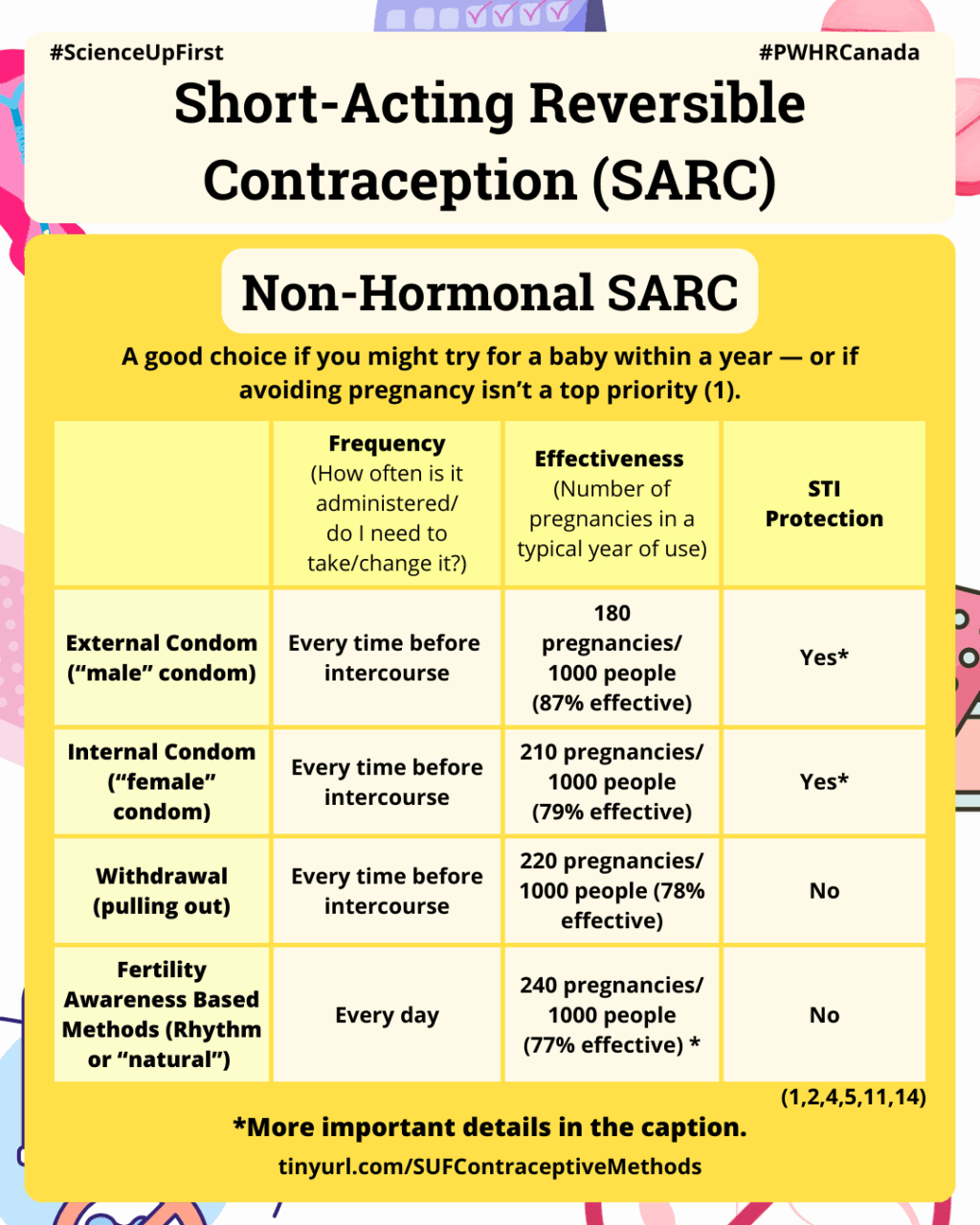
Short-Acting Reversible Contraception (SARC)
A good option if you want to become pregnant within the next year – or if you are not actively planning a pregnancy, but would be okay if you became pregnant (1).
Hormonal SARC
Injectable Contraception (4,5,8,11,14,15,16)
Frequency: Every 3 months (four times a year).
Effectiveness with typical use: 60 pregnancies per 1000 people in a year (96% effective).
What: An injection in your arm or upper buttocks.
How: The injected progestin prevents ovulation – if no ovule is released, there can’t be a pregnancy – and thickens the cervical mucus, which acts as a physical barrier and makes it harder for sperm to reach an ovule.
STI protection: No
Reversible: Yes, but fertility can take a year or more after the last injection to return to normal.
Oral contraceptive pill (1,4,5,11,17)
Frequency: Taken every day at the same time.
Effectiveness with typical use: 90 pregnancies per 1000 people in a year (93% effective).
What: A small pill that either contains 2 hormones (estrogen and progestin) or only progestin (mini Pill).
How: Hormone·s from the pill prevent ovulation and thickens the cervical mucus.
STI protection: No
Reversible: Yes
Contraceptive patch (1,4,5,11,18)
Frequency: Replaced every week.
Effectiveness with typical use: 90 pregnancies per 1000 people in a year (93% effective).
What: A thin plastic patch that you stick on your buttock, upper outer arm, lower abdomen or upper body.
How: Slowly releases progestin and estrogen to prevent ovulation and thicken the cervical mucus.
STI protection: No
Reversible: Yes
Vaginal ring (1,4,5,11,19)
Frequency: Replaced every month.
Effectiveness with typical use: 90 pregnancies per 1000 people in a year (93% effective).
What: A thin flexible ring inserted in your vagina.
How: Slowly releases progestin and estrogen to prevent ovulation and thicken your cervical mucus.
STI protection: No
Reversible: Yes
Non-Hormonal SARC
External (“male”) Condom (1,4,7,8)
Frequency: Every sexual intercourse.
Effectiveness with typical use: 180 pregnancies per 1000 people in a year (87% effective)
What: A thin membrane, usually made of latex, worn over an erect penis.
How: Catches semen so sperm doesn’t enter the vagina.
STI protection: Yes, but not against all STIs. STIs that are transmitted through skin to skin contact (e.g. genital herpes, genital warts) can still be contracted even with condom use.
Reversible: Yes
Internal (“female”) Condom (1,4)
Frequency: Every sexual intercourse.
Effectiveness with typical use: 210 pregnancies per 1000 people in a year (79% effective).
What: A non-latex pouch that is inserted in the vagina up to 4 hours before sex.
How: Catch the semen so sperm doesn’t enter the vagina.
STI protection: Yes, but not against all STIs. STIs that are transmitted through skin to skin contact (e.g. genital herpes, genital warts) can still be contracted even with condom use.
Reversible: Yes
Withdrawal (pulling out) (1,4)
Frequency: Every sexual intercourse.
Effectiveness with typical use: 220 pregnancies per 1000 people in a year (81% effective)
What: The penis is pulled out of the vagina before cumming, away from the vagina and vulva.
How: Prevent sperm from entering the vagina.
STI protection: No.
Reversible: Yes
Fertility Based Awareness Methods, also called “Rhythm” or Natural Birth Control Methods (1,4,7)
Frequency: Every day.
Effectiveness with typical use: 240 pregnancies per 1000 people in a year (77% effective).
What: Consist of keeping track of your cycle by checking your basal (waking) body temperature and cervical mucus daily in order to determine your fertile window.
How: Avoid vaginal sex or use a barrier method (condom) when you are fertile to avoid pregnancy.
STI protection: No.
Spermicide (7,15,20,21,22)
Frequency: Every sexual intercourse.
Effectiveness with typical use: 210 pregnancies per 1000 people in a year (79% effective). It is one of the least effective forms of birth control and thus, should be used in combination with other contraception methods.
What: a foam or film inserted in the vagina and deposited in front of the cervix at least 15 minutes before having sex. The spermicide is only effective for about one hour, hence it will need to be reapplied frequently, which can cause irritation and make you more vulnerable to various STIs – simultaneous condom use is recommended.
How: the active ingredient in spermicide, nonoxynol-9, works by killing sperm cells before they can reach the ovule.
STI protection: No, and spermicide can increase the risk of HIV and other STIs transmission.
Reversible: Yes
Sponge (15,23)
Frequency: Every sexual intercourse.
Effectiveness with typical use: 240 pregnancies per 1000 people in a year (76% effective) in people who have previously given birth. 120 pregnancies per 1000 people in a year (88% effective) in people who have not given birth.
What: a soft sponge with spermicide that must be wet before being placed in the vagina to cover the cervix. It can be inserted up to 24 hours before sex and must stay in for at least 6 hours after – but no more than 30 hours total. It is single-use and can’t be removed and reinserted.
How: The sponge acts as a physical barrier that prevents sperm from entering the uterus, while the spermicide kills the sperm.
STI protection: No, and spermicide use can increase the risk of HIV and other STIs transmission.
Reversible: Yes
Cervical cap and Diaphragm (7,15,24)
Frequency: Every sexual intercourse.
Effectiveness with typical use: Cervical cap: 220 pregnancies per 1000 people in a year (78% percent effective). Diaphragm: 170 pregnancies per 1000 people in a year (83% effective).
What: a small, soft cup placed over the cervix along with a spermicide. They can be inserted up to 2 hours before sex and must be left in place for at least 6 hours after, but not longer than 24 hours. The gel must be reapplied before each subsequent intercourse or every 2 hours.
How: Act as a physical barrier that prevents sperm from entering the uterus.
STI protection: No, and spermicide use can increase the risk of HIV and other STIs transmission.
Reversible: Yes
Choosing what’s right for you
There are lots of contraception options in Canada.
Some you use daily, others last for years.
Some use hormones, some do not (1,2,3,4,8).
It all depends on your goals and what works best for you.
And remember — condoms are the only contraceptive method that can help protect against multiple STIs (4).
- Which Birth Control Method is Right for You? | The Society of Obstetrician and Gynaecologists of Canada | 2015
- Contraception | The Society of Obstetrician and Gynaecologists of Canada
- Birth Control Methods & Options | Planned Parenthood
- Birth Control Options | Planned Parenthood Toronto; PDF: Birth Control Options | Planned Parenthood Toronto
- How well contraception works at preventing pregnancy | NHS
- Hormonal IUD | Planned Parenthood Toronto
- Effectiveness of Birth Control Methods | The American College of Obstetricians and Gynecologists (ACOG)
- It’s a plan – Helping you make decisions about contraception | The Society of Obstetrician and Gynaecologists of Canada
- Birth Control Implant | Planned Parenthood
- What are hormonal IUDs? | Planned Parenthood
- What are the different types of contraception? | National Institute of Child Health and Human Development (NICHD)
- Birth Control | FDA | Current as of October 2024
- What are non-hormonal IUDs? | Planned Parenthood
- Birth Control Shot | Planned Parenthood
- Contraception | The society of Obstetricians and Gynaecologists of Canada
- Contraceptive Injection (Depo Provera) | Halifax Sexual Health Centre
- Birth Control Pill | Planned Parenthood
- Birth Control Patch | Planned Parenthood
- Birth Control Ring | Planned Parenthood
- Vaginal Spermicides | My Health Alberta
- What are the disadvantages of using spermicide? | Planned Parenthood
- How do I use spermicide? | Planned Parenthood
- How do I use the sponge? | Planned Parenthood
- Diaphragm | My Health Alberta
Share our original Bluesky Post!
Several methods of contraception exist in Canada: the choice depends on your needs. Some facts to remember 👇 -The fertility method ≠ protection -Only condoms (partially) protect against STIs -Some methods expire! Learn more here: tinyurl.com/SUFContraceptiveMethods @pwhrcanada.bsky.social
— ScienceUpFirst (@scienceupfirst.bsky.social) September 25, 2025 at 3:18 PM
[image or embed]
View our original Instagram Post!